How to Memorize the H’s and T’s of ACLS
SUDDEN CARDIAC ARREST, or SCA, is defined as “a sudden and unexpected pulseless condition attributed to cessation of cardiac mechanical activity”, according to the Sudden Cardiac Arrest Foundation. SCA is the leading cause of death in adults over the age of 40 in the United States, but fortunately is often reversible and can be treated with early intervention.
Understanding what protocols and actions to take when a patient is experiencing cardiac arrest is a crucial part of Advanced Cardiac Life Support (ACLS).
They are complex, so practitioners and teachers have developed a mnemonic device, known as the “H’s and T’s of ACLS”, which explain the conditions associated with pre‐arrest and cardiac arrest algorithms.
Because many cardiac arrest conditions are reversible, determining and treating the cause is a must for optimal patient care and outcome. Here are the H’s and T’s of ACLS from the latest American Heart Association standards and guidelines and AMC.
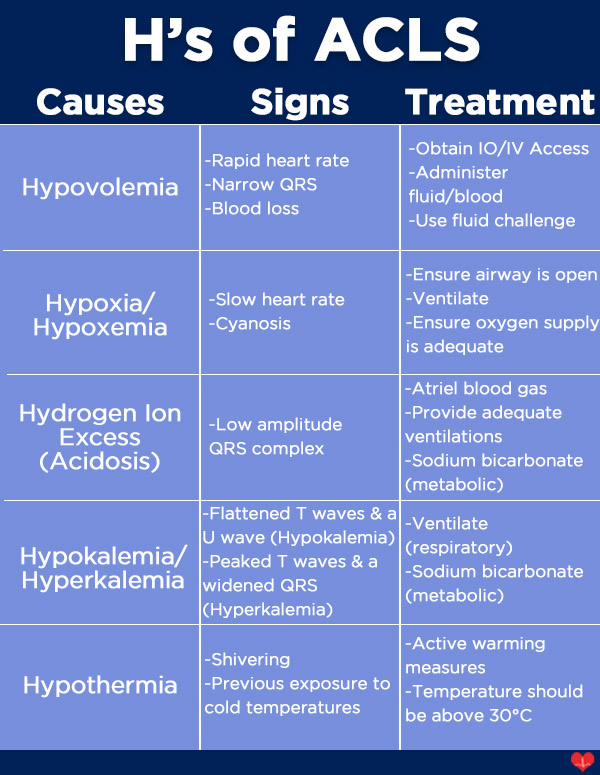
What are the "H's"?
Hypovolemia
Hypovolemia is a common cause of cardiac arrest and develops from severe fluid or blood loss. This is typically a result of excessive sweating, vomiting, traumatic blood loss, severe burns or diarrhea.
Hypoxia or Hypoxemia
Hypoxia is an insufficiency in the amount of oxygen that reaches vital organs and tissues. It can occur from several reasons, including disorders of the lungs, drowning, fires, high altitudes, chemical or gas poisonings, etc.
Hydrogen Ion Excess (or Acidosis)
Hydrogen Ion Excess, or Acidosis, is either a respiratory or metabolic emergency that can lead to cardiac arrest when there are inadequate pH levels caused by too much acid in the body. Some causes of acidosis include lung disease, CO2 buildup, DKA/AKA, liver failure, and cancer.
Hypokalemia and Hyperkalemia
Both hypokalemia and hyperkalemia are conditions in which potassium levels are too low or too high to maintain normal contraction of the myocardium. When these levels of K+ are off, the individual is at high risk for cardiac arrest. A few causes include the use of diuretics, excessive vomiting, DKA, and kidney disease or failure. Hyperkalemia may also be caused by diabetes, kidney disease, or as a side effect of certain drugs.
Hypothermia
Hypothermia occurs when the body cannot keep itself warm and the core temperature drops below 30 degrees Celsius. It can lead to cardiac arrest because cardiac output is decreased. This condition ensues when an individual is exposed to extreme or prolonged cold weather or water temperatures.
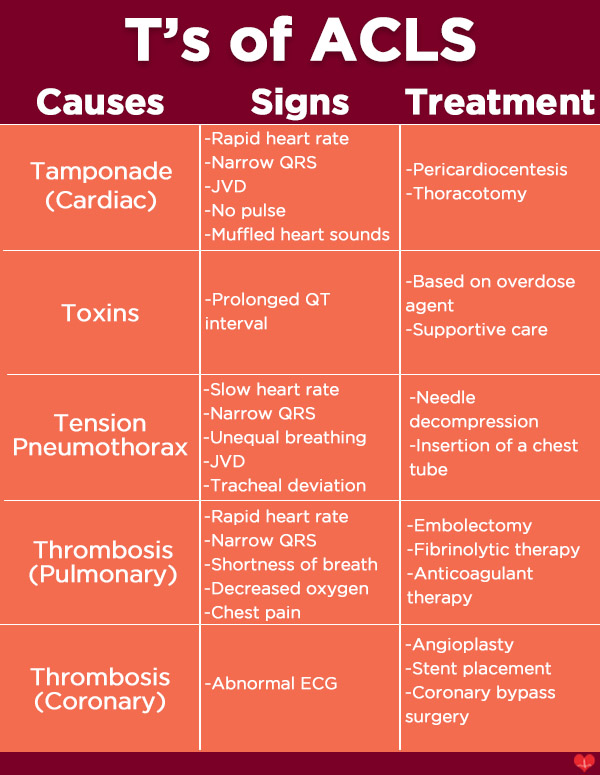
Tamponade (Cardiac)
Cardiac tamponade is a buildup of blood or fluid in the pericardial space, causing pressure on the heart and preventing the ventricles from filling properly. Causes include chest trauma, pericarditis, and myocardial rupture.
Toxins
The ingestion of toxins is one of the most common causes of cardiac arrest and occurs when an individual intentionally or unintentionally overdoses on medication, street drugs, or chemical substances. One commonly seen sign of cardiac arrest due to toxins is a prolonged QT interval.
Tension Pneumothorax
Tension pneumothorax develops when air accumulates in the pleural cavity without an outlet. This buildup causes a shift in the mediastinum, blocking venous return to the heart and potentially resulting in cardiac arrest. Common causes include chest trauma, iatrogenic injury, and mechanical ventilation. Signs include unequal breath sounds, jugular venous distension, ventilation issues, and tracheal deviation.
Thrombosis (Pulmonary)
Thrombosis, or a pulmonary embolism, typically develops after a blood clot forms in another area of the body and can lead to cardiac arrest in some instances. A pulmonary embolism is a blockage of the lung’s main artery caused by blood clots.
Thrombosis (Coronary)
Coronary thrombosis is a blockage within one or more coronary arteries due to clotted blood, which prevents blood from properly flowing to the heart. This may cause cardiac arrest depending on the intensity and location of the blockage, and is often associated with myocardial infarction.
What are the "H's"?
Tamponade (Cardiac)
Cardiac tamponade is a buildup of blood or fluid in the pericardial space that causes pressure on the heart, preventing proper ventricular filling. Causes include chest trauma, pericarditis, and myocardial rupture.
Toxins
The ingestion of toxins is one of the most common causes of cardiac arrest, occurring when an individual intentionally or unintentionally overdoses on medication, street drugs, or chemicals. A prolonged QT interval is a common sign of toxin‐induced cardiac arrest.
Tension Pneumothorax
Tension pneumothorax develops when air becomes trapped in the pleural cavity with no exit, leading to mediastinal shift and blocked venous return to the heart. This condition may result from chest trauma, iatrogenic factors, or mechanical ventilation, and presents with unequal breath sounds, jugular venous distension, ventilation issues, and tracheal deviation.
Thrombosis (Pulmonary)
Thrombosis, or pulmonary embolism, typically develops after a blood clot forms elsewhere in the body and subsequently blocks the lung’s main artery, potentially leading to cardiac arrest.
Thrombosis (Coronary)
Coronary thrombosis is the blockage of one or more coronary arteries due to clotted blood, which prevents adequate blood flow to the heart and may cause cardiac arrest depending on the severity and location of the blockage. It is often associated with myocardial infarction.
Additional resources to help you achieve ACLS success:
We offer online ACLS certification and ACLS renewal, click here to learn more!

