- ACLS BLS for Adults
- Initiating the Chain of Survival
- 2020 BLS Guideline Changes
- One Rescuer Adult BLS CPR
- Two Rescuer Adult BLS CPR
- Adult Mouth-to-Mask and Bag-Mask Ventilation
- Adult Basic Life Support (BLS) Algorithm
- BLS for Children/Infants
- CPR Steps for Children
- One-Rescuer BLS/CPR for Infant (newborn to age 12 months)
- CPR Steps for Infants
- Child/Infant Mouth-to-Mouth Ventilation
- Systems Of Care
- Cardiopulmonary Resuscitation
- Post-Cardiac Arrest Care
- Acute Coronary Syndrome
- Acute Stroke
- The Resuscitation Team
- Education, Implementation, Teams
- ACLS Cases Respiratory Arrest
- Pulseless Ventricular Tachycardia and Ventricular Fibrillation
- Pulseless Electrical Activity Asystole
- Adult Cardiac Arrest Algorithm
- Post-Cardiac Arrest Care
- Adult Immediate Post-Cardiac Arrest Care Algorithm
- Symptomatic Bradycardia
- Adult Bradycardia with Pulse Algorithm
- Tachycardia
- Stable And Unstable Tachycardia
- Adult Tachycardia With Pulse Algorithm
- Acute Coronary Syndrome
- Acute Coronary Syndrome Algorithm
- Acute Stroke
- Acute Stroke Algorithm
Education, Implementation, Teams
Only about 20% of people that have a cardiac arrest inside a hospital will survive. This statistic prompted the development of a Cardiac Arrest System of Care. Four out of five patients with cardiopulmonary arrest have changes in vital signs prior to the arrest. Therefore, most patients that eventually have a cardiac arrest showed signs of impending cardiac arrest. Survival rates could be improved if patients are identified and treated with ACLS protocols sooner.
Originally, specialized groups of responders within a hospital, called Cardiac Arrest Teams, attended to a patient with recognized cardiac arrest. These teams responded to a “Code Blue” after someone presumably recognized an active cardiac arrest and sought help. Many believed Cardiac Arrest Teams would improve patient survival, but the results were disappointing. Studies show that survival rates were the same in hospitals with Cardiac Arrest Teams as in those without a team. As a result, hospitals are replacing Cardiac Arrest Teams with Rapid Response Teams (RRTs) or Medical Emergency Teams (METs). Anyone can call for the RRT/ MET if there is any concern by the patient, a health care provider, or a family member.
Rather than waiting for the loss of consciousness and full cardiopulmonary arrest, RRTs/METs closely monitor patients in order to treat patients before the cardiac arrest occurs. These teams combine the efforts of nurses, physicians, and family members to detect an impending cardiac arrest.
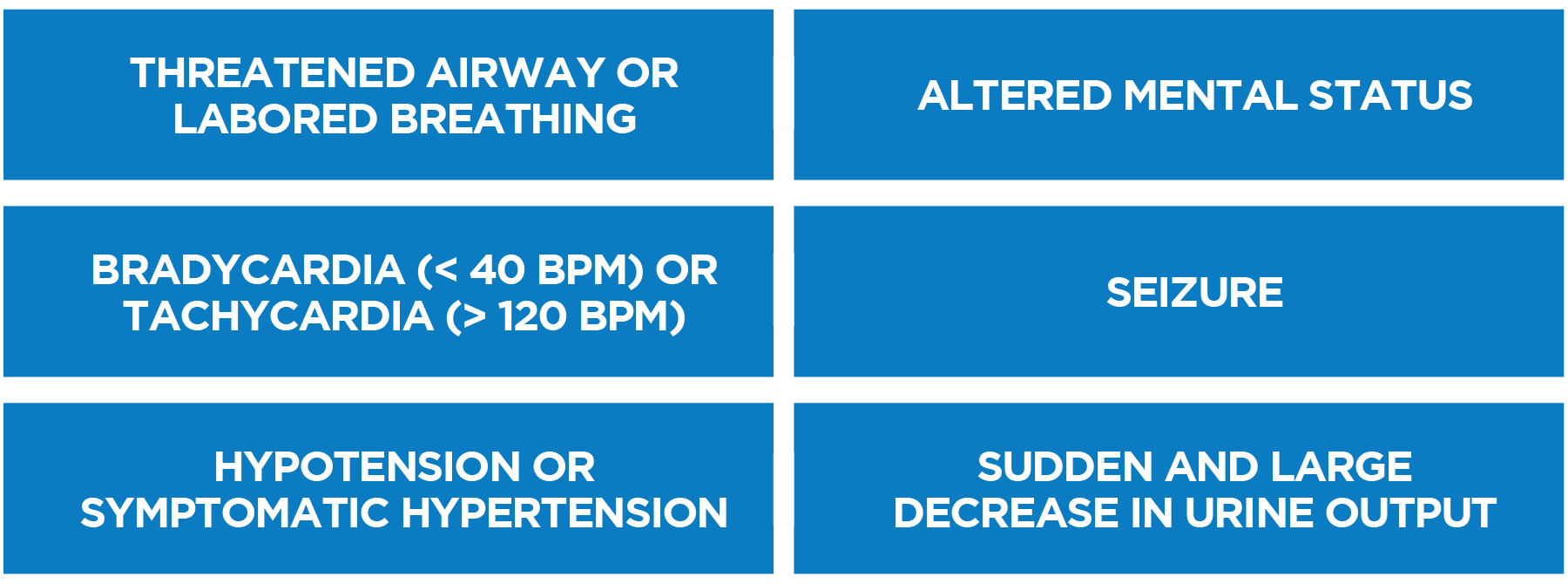
RRT/MET ALERT CRITERIA
When hospitals implement RRTs/METs, there are fewer cardiac arrests, fewer ICU transfers, improved survival rates, and shorter lengths of inpatient stay.
